Barriers To ME/CFS Research : Why Its Taking So Long To Study ME

Derailment By The Biopsychosocial Model
The BPS model created in the 80s by Simon Wessley and propelled to mainstream popularity by the fraudulent PACE trial has left a whole generation of doctors who believe "Chronic Fatigue Syndrome" is a psychiatric condition and Myalgic Encephalomyelitis non-existent.
Despite the fact that the WHO has always categorized ME as a post-viral neuroimmunological disorder, the prevalence of this idea that ME/CFS is caused by "false illness beliefs" leading to deconditioning has led to a complete lack of research and funding investigating the biological realities of the disease. Major guidelines were not changed until 2020 leading to research decades behind where it should be and prominent studies are still being influenced by this disproven theory.
—-
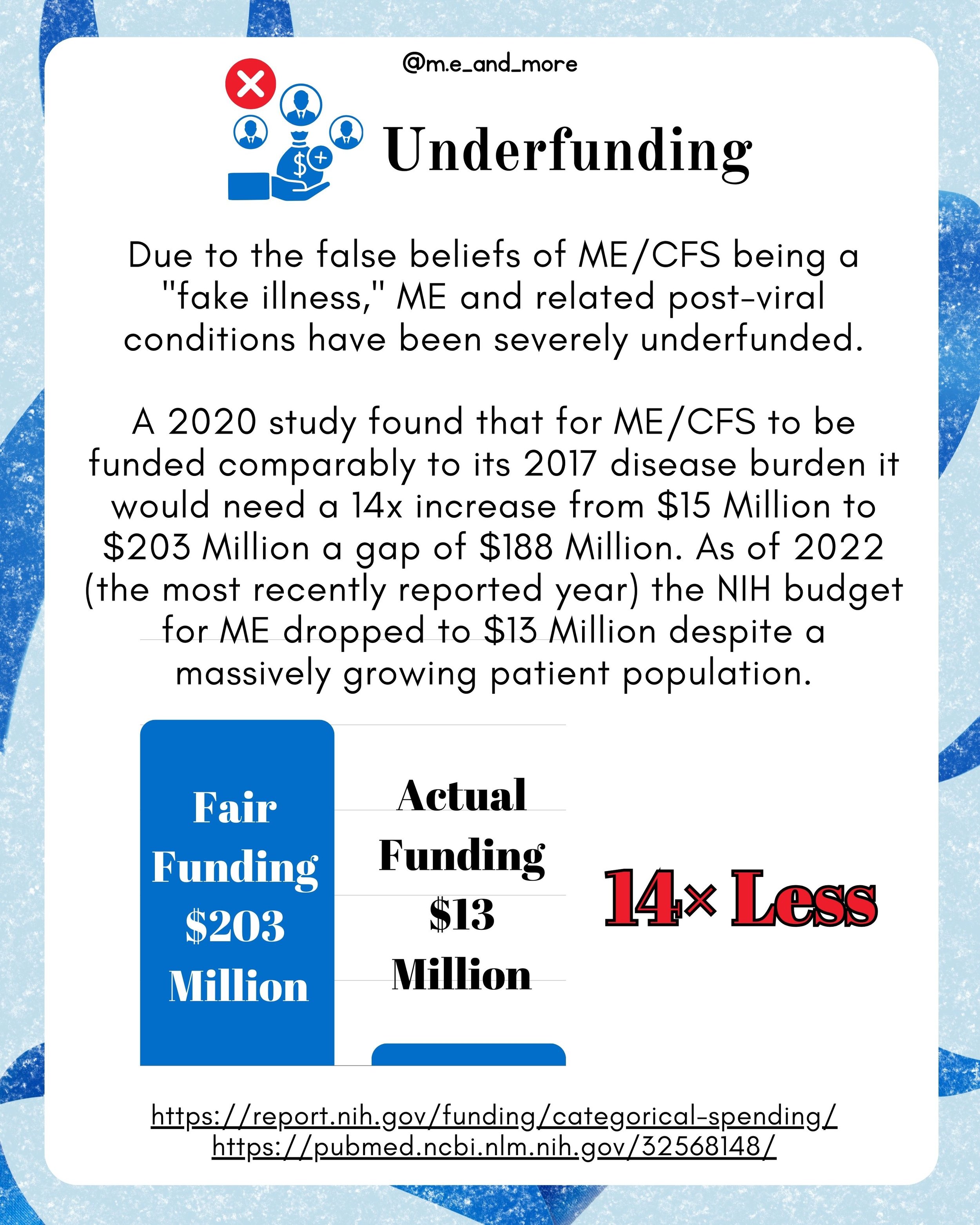
Underfunding
Due to the false beliefs of ME/CFS being a "fake illness," ME and related post viral conditions have been severely underfunded.
A 2020 study found that for ME/CFS to be funded comperably to its 2017 disease burden it would need a 14x increase from $15 Million to $203 Million a gap of $188 Million. As of 2022 (the most recently reported year) the NIH budget for ME dropped to $13 Million despite a massively growing patient population.
While the $77 Million dollars given to PASC including long covid greatly increased research in the general area of ME/CFS, this comes with its own disease burden as yet unmeasured. All NIH funding in 2022 for ME and Long Covid combined still is over 2x less than the burden proportionate funding for the #millionsMissing with ME alone in 2017.
https://report.nih.gov/funding/categorical-spending/
—-
Poor Disease Definition
There are numerous definitions of ME, CFS and ME/CFS. Historically, many definitions used in research did not require the cardinal symptom of post-exertional malaise (PEM) or post-exertional neuroimmune exhaustion (PENE).
This has led to many studies including unknown numbers of patients who do not have ME but have only idiopathic chronic fatigue, fibromyalgia, depression or other fatiguing illnesses that may respond drastically different to treatment and especially exercise.
Long covid studies often suffer the same diagnostic difficulties with patients suffering acute lung damage being grouped together with patients suffering post-viral ME/CFS.
The International Consensus Criteria created in 2016 aim to provide a much stricter research definition for ME requiring PENE, neurological, gastro immunological, and cardiac/metabolic symptoms.
—-
Lack Of Access To Severe Patients
Many studies that aim to draw conclusions about ME are done at research universities or medical institutions. However, 25% of patients with ME are housebound or bedbound. These patients are therefore excluded from in-person studies.
Additionally, some studies may require physical tasks like walking or biking which are not possible for more severe patients.
Severe patients have the most prominent dysfunction and often respond differently to treatment or cannot tolerate treatment that benefits less severe patients. Therefore excluding these patients has the possibility to produce inaccurate results.
Severe patients can be included in research by doing home visit studies or virtual studies and allowing a caregiver to fill in as much of the paperwork as possible. Severe patients should be studied as an important subgroup that may require different interventions.
—-
Long Covid Reinventing The Wheel
In comparison to the meager funding for ME, $1.15 Billion dollars went to the RECOVER Initiative for Long Covid. Why then has this funding not produced more results?
While Long Covid is not identical to ME and patients with long covid face unique challenges, aproximately 50% of long covid patients also have ME.
Therefore, it is extremely frustrating to see much funding simply reproducing the same exercise intolerance studies we have done already in ME. The results of these studies are predictable and move us no closer to treatment or diagnostic testing. Simply knowing that Long Covid patients have ME, brings us no closer to helping either group.
While it is promising to see governments funding long covid studies, it is disappointing when the studies they choose simply repeat disproving the damaging psychological theory of the illness.
—-
Gap Between Treatment & Investigative Studies
There are two types of studies in researching a novel (which ME is due to decades of underfunding) disease.
Investigative studies look at as many biomarkers as possible to provide the clues used to develop theories of the disease.
Treatment-driven studies test new or already approved drugs for efficacy against the disease.
Many patients argue over whether we need more investigative or treatment-driven studies. The answer is we need both.
Investigative studies must be done with the intention to find biomarkers that can be treated or indicate treatment pathways.
Treatment-driven studies must choose the treatments to trial based on theories compatible with investigative results.
This is why communication between researchers and research teams is essential to the progression of ME understanding and treatment. The scientific method has no room for ego.
—-
Solutions
To drive research into ME forward we must
1.) Recruit a well-defined sample of patients including all levels of severity and only including those who experience post-exertional malaise.
2.) Test new hypotheses within a framework that looks towards understanding the illness in ways we have not yet investigated.
3.) Trial new and more importantly pre-existing drugs in double-blind studies to find immediately actionable treatments.
4.) Dismiss the flawed psychologization of ME and lobby governments to provide fair funding of an order of magnitude increase to this devastating illness.
—-
How Initiative Can Help
One of the major barriers to studying ME is the cost associated with recruiting patients. Due to underfunding and the difficulty with screening patients properly and including severe patients in research, many studies struggle to get off the ground.
The StudyME initiative is a project by the Open Medicine Foundation that aims to increase enrollment in ME scientific research by building a database of patients that researchers can quickly contact when new studies are deployed. This increases sample size, reliability, and research into ME while lowering costs for researchers. Other similar initiatives include the Solve ME registry which likewise is a central recruitment hub for studies.
Signing up takes on a few minutes at www.omf.ngo/studyme/
—-
The Need For Collective Action
For patients with ME, it can feel like research is going nowhere. Decades of wasted potential from the psychologization of a biomedical disease has put us miles behind research into similar conditions like MS. Underfunding means the studies we do get are often underwhelming.
I hope that understanding the barriers researchers face can help our community to understand why research is taking so long and help us take steps to address it. Collectively we spend massive quantities of money on unproven treatments and supplements. If we all spent our money on research instead it would benefit everyone.
Unfortunately, we each have an individual incentive to try anything to improve, and there are endless traps of scam artists and snake oil to waste money on.
I encourage all people with ME to look at our disease from a collective perspective and do what you can to advance research and advocacy. Because individually our chances of recovery are not good, but collectively this is a problem we can solve.
—-
MECFS Research faces an uphill battle if we are to cure this life destroying condition. While organizations like @openmedf are working hard to solve Myalgic Encephalomyelitis aka MECFS, it is important that the community understands the barriers to research so that we can overcome them.
The name Chronic Fatigue Syndrome and the Biopsychosocial Model of Myalgic Encephalomyelitis derailed research in the 80s and it has only gotten back on track on a large scale since the development of long Covid and massive advocate action to change NICE and Mayo Clinic guidelines in 2020. That means compared with simular illnesses like MS we are 40 years behind!
Furthermore, funding for ME and related complex Chronic Illness is abysmal. It is one of the most underfunded diseases in comparison to patient burden requiring a 14x increase and increase of $188 million to recieve proper funding.
There is great difficulty in recruiting patients with severe ME whose profound dysfunction and differences in symptoms and functioning are essential to study.
Many desperate people within the community feel hopeless about research and prioritizing buying experimental or snake oil treatments as opposed to investing in collective studies that could benefit us all with evidence based recommendations.
I believe it is essential that patients understand why research for ME is so difficult. Only then can we take steps to change the pace of progress.
One such step I have partnered with Open Medicine Foundation to promote is their Study ME initiative which aims to connect patients researchers to decrease the cost of study recruitment leaving more of our limited funds available for research. To enroll simply go to www.omf.ngo/studyme/
The more research we are able to fund and participate in the faster we will be able to Solve ME and return from this living Death. If your loved one has ME understand that it is not for lack of trying that they do not get better. It is for lack of research.
Evidence based medicine fails pwME because we lack evidence. Instead of putting pressure on your loved one for what they can't control put pressure on your government to fund ME/CFS or donate to orgs like OMF directly.