Fibromyalgia and MECFS… Differentiation and Treating Comorbid Patients.
Connected But Different
ME and fibro are deeply connected diseases. There is massive overlap between the two populations to the extent that many doctors do not know the difference between these diseases and treat all patients with either or both equivalently (aka poorly).
However, distinguishing between these 3 groups (Primarily ME, Primarily Fibro, ME & Fibro) is absolutely essential to providing appropriate medical treatment. I use the term primarily here because many patients who qualify for both diagnoses have significantly worse symptoms associated with one and respond best when treated primarily for that diagnosis.
This post will help you learn to distinguish between these three groups and react accordingly. It will focus primarily on identifying and differentiating fibromyalgia in patients who know whether they have MECFS. For more information about diagnosing MECFS please see my post on the MECFS International Consensus Criteria.
----
Fibromyalgia
Fibromyalgia is an autoimmune disease that causes severe pain as well as fatigue, sleep disturbance and cognitive dysfunction.
As of 2016, the revised diagnostic criteria for fibromyalgia are:
(1)
Generalized pain, defined as pain in at least 4 of 5 regions, left and right upper and lower as well as axial (along your spine)
(2)
Symptoms have been present at a similar level for at least 3 months.
(3)
Widespread pain index (WPI) ≥ 7 and symptom severity scale (SSS) score ≥ 5 OR WPI of 4–6 and SSS score ≥ 9.
(4)
A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
----
The Other Wastebasket
As I discuss in my post "Chronic Fatigue Syndrome; Why every use of this wastebasket diagnosis has to go." CFS is often used by lazy doctors as a way to dismiss patients with complex chronic illness symptoms and no positive lab test results. Fibromyalgia is often used identically. See "Rheumatologists & MECFS; Why They Get It So Wrong" for more info.
This is a huge problem, because many fibromyalgia patients respond very positively to exercise including GET. However, MECFS patients are significantly harmed by the same therapy. Therefore being thrown into the wrong wastebasket is even more harmful than being given a wastebasket diagnosis already is.
It is important that doctors and patients are aware of the difference between fibromyalgia, MECFS, and idiopathic (unexplained) chronic fatigue. These are not the same diagnoses and only by correctly identifying each and can appropriate treatment be provided. MECFS and Fibro are both no longer considered diagnoses of exclusion meaning they are valid regardless of other comorbidities.
----
Different Key Features
The most important thing to note about these two diagnoses is that the key diagnostic symptom is different. For fibro, widespread debilitating pain is the necessary symptom. For MECFS it is post-exertional malaise. While most of the symptoms overlap, it is important that these two diagnostic symptoms be prioritized when it comes to diagnosis and treatment because the relative importance of these symptoms greatly changes the patients' response to treatment.
Chronic fatigue is a symptom of both fibro and ME. Chronic fatigue in fibro can be extremely debilitating and just as severe as in some ME patients. However, if a patient does not experience PEM than it is still inappropriate to diagnose them with CFS or MECFS. This is because as long as they do not experience PEM they may likely benefit from exercise.
Crucially, chronic fatigue outside of patients meeting the criteria for fibro or MECFS should not be diagnosed as CFS, MECFS, ME, or fibro. It should be diagnosed as idiopathic chronic fatigue and investigated until an actual diagnosis can be made. While being undiagnosed is not fun, it is much more harmful to be given an incorrect diagnosis.
-----
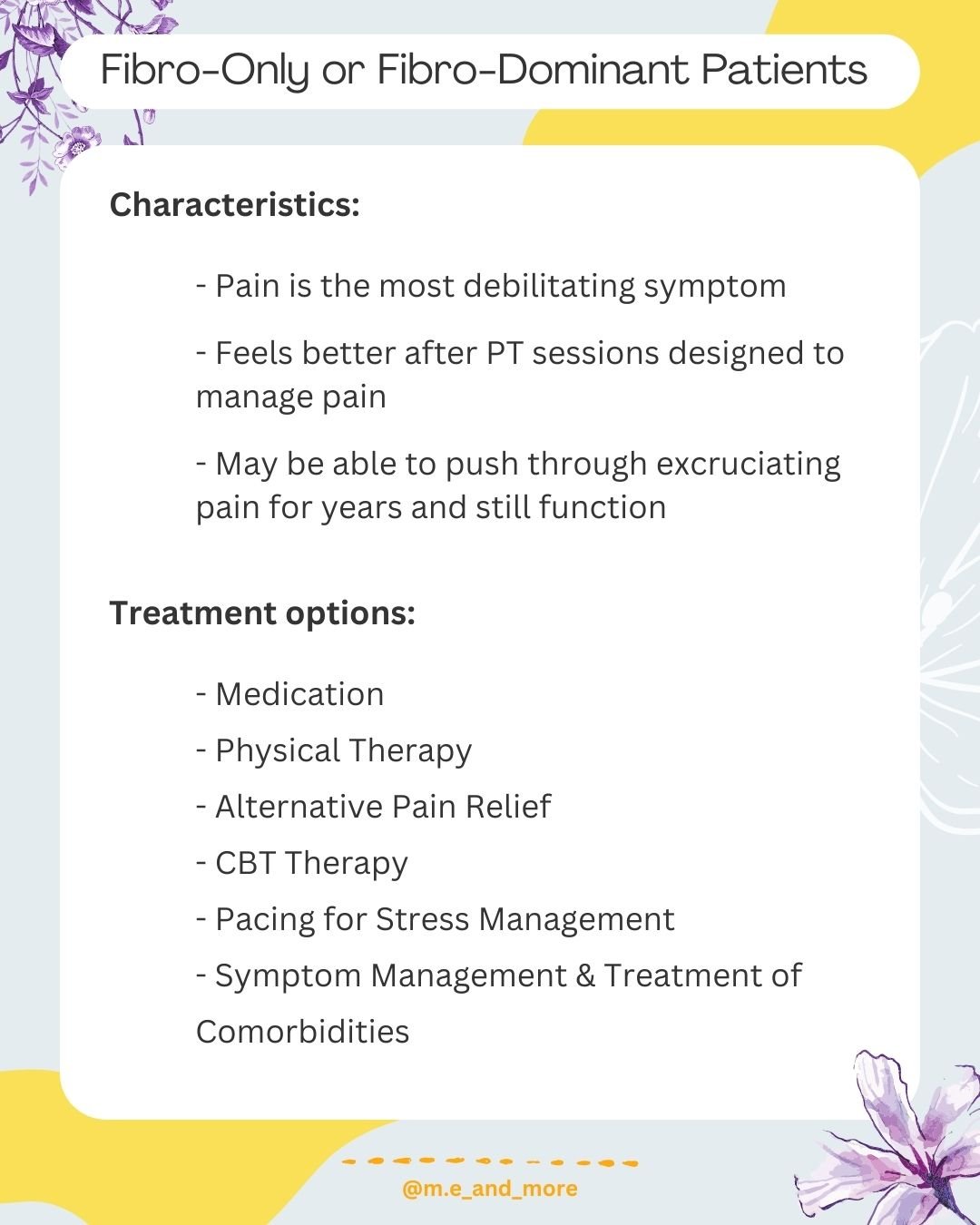
Fibro Only or Fibro Dominant Patients
Characteristics:
-Pain is most debilitating symptom
-Feels better after PT sessions designed to manage pain
-May be able to push through excruciating pain for years and still function
Treatment options:
-Medication
-Physical Therapy
-Alternative Pain Relief
-CBT Therapy
-Pacing for Stress Management
-Symptom Management & Treatment of Comorbidities
----
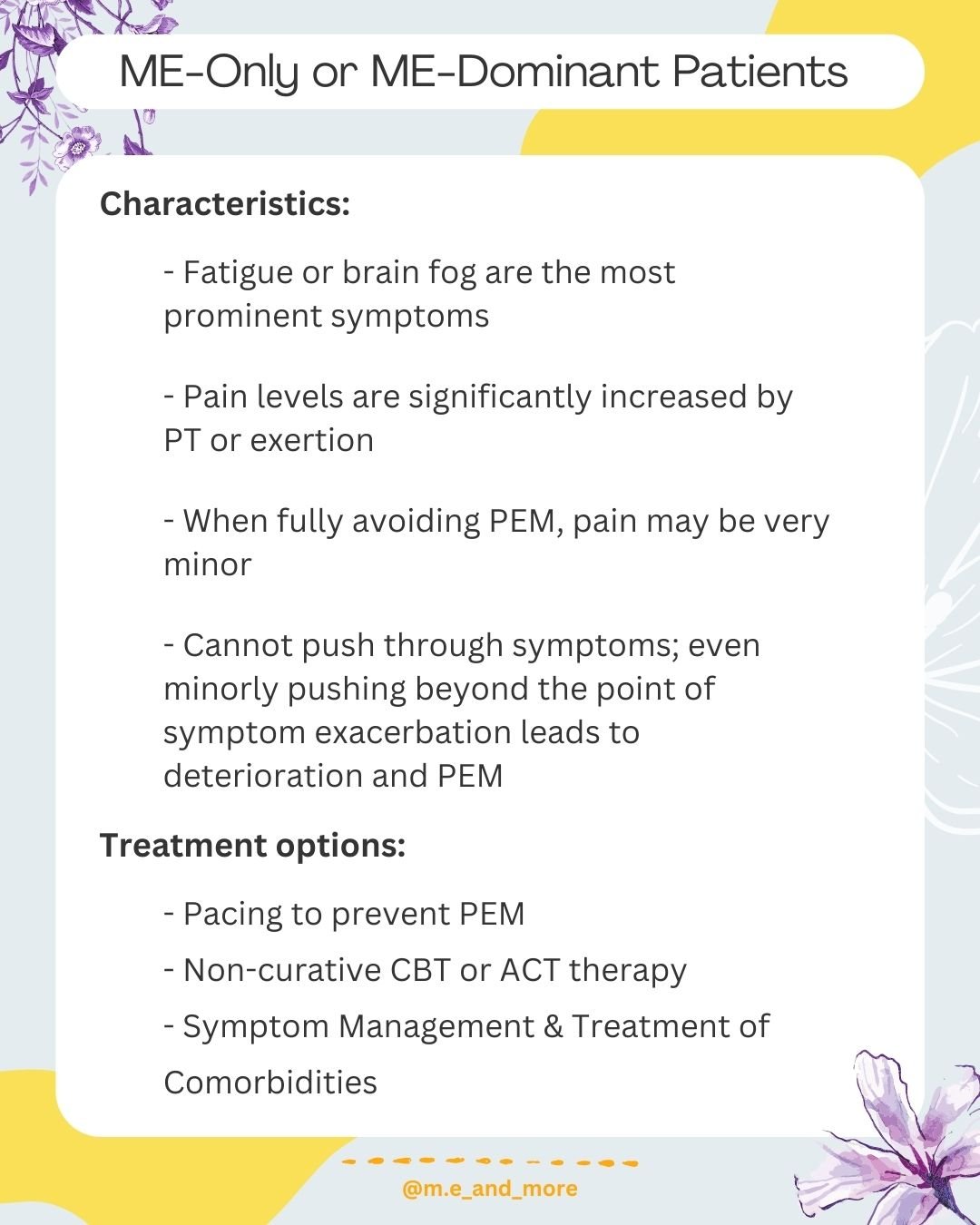
ME Only or ME Dominant Patients
Characteristics:
-Fatigue or brain fog is most prominent symptoms
-Pain levels significantly increased by PT or exertion
-When fully avoiding PEM pain may be very minor
-Cannot push through symptoms, even minorly pushing beyond the point of symptom exacerbation leads to deterioration and PEM
Treatment Options:
-Pacing To Prevent PEM
-Non-curative CBT or ACT therapy
-Symptom Management & Treatment of Comorbidities
----
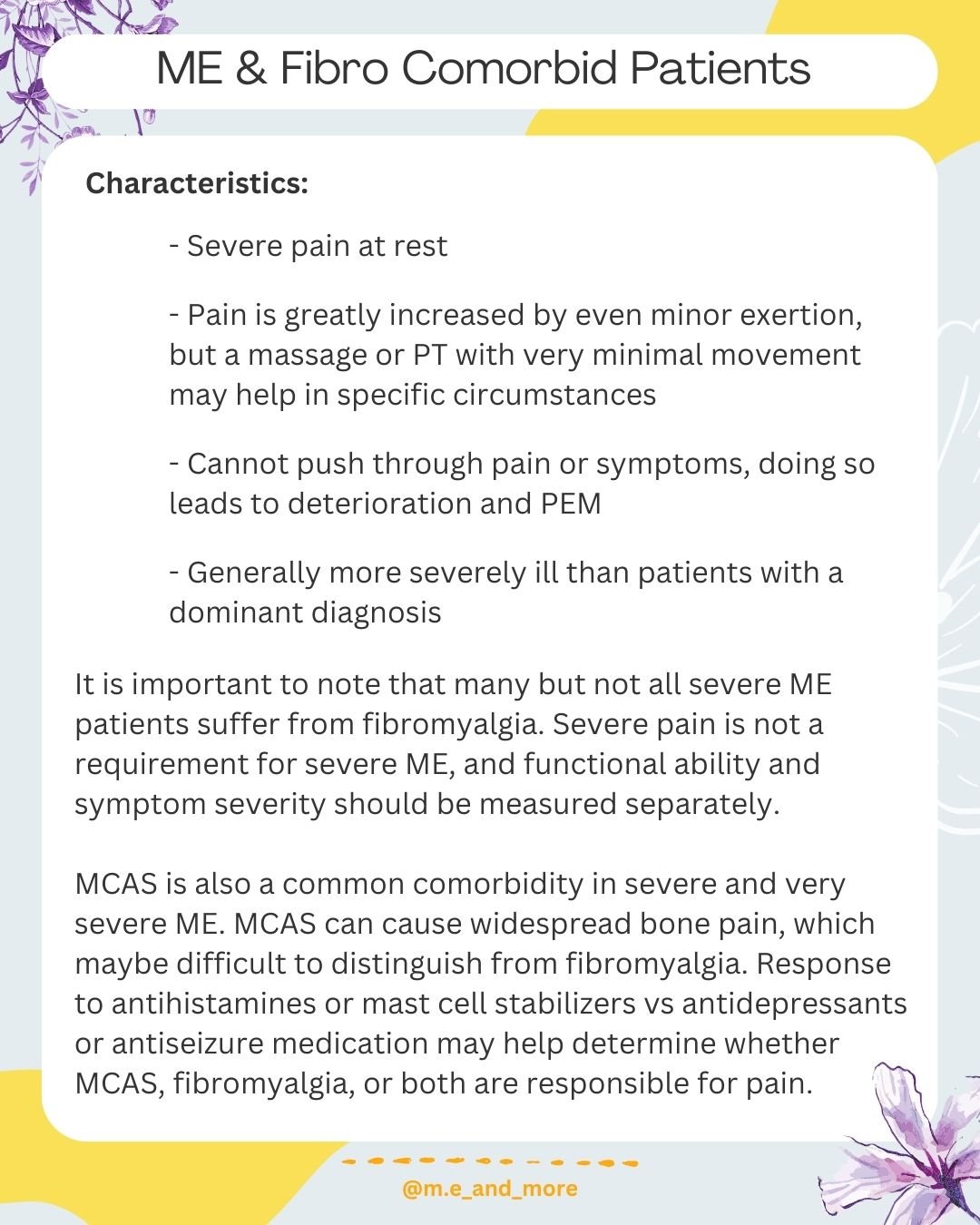
ME & Fibro Comorbid Patients
Characteristics:
-Severe pain at rest
-Pain is greatly increased by even minor exertion, but massage or PT with very minimal movement may help in specific circumstances
-Cannot push through pain or symptoms, doing so leads to deterioration and PEM
-Generally more severely ill than patients with a dominant diagnosis
It is important to note that many but not all severe ME patients suffer from fibromyalgia. Severe pain is not a requirement for severe ME and functional ability and symptom severity should be measured separately.
MCAS is also a common comorbidity in severe and very severe ME. MCAS can cause widespread bone pain which may be difficult to distinguish from fibromyalgia. Response to antihistamines or mast cell stabilizers vs antidepressants or antiseizure medication may help determine whether MCAS, fibromyalgia or both are responsible for pain.
----
Medication Considerations in Comorbid Patients
In patients with MECFS, it is important that pain management be prioritized to maximize sleep and minimize pain-related exertion. It is also essential that the prescribing doctor understands the inability of ME patients to complete physical therapy and that this is a necessary boundary to avoid permanently worsening their condition.
Many patients with severe ME are very sensitive to medication. Therefore compounded low-dose medications may be better tolerated than traditional therapies.
Medication specifics:
LDN: The evidence for LDN is increasingly powerful. LDN can reduce both pain and fatigue in fibromyalgia and has increasing evidence in MECFS.
PEA: Is a supplement that has shown significant evidence for helping manage pain in fibromyalgia. It is well tolerated by MECFS patients.
Lyrica: Pregabalin is a nerve pain and anti-seizure medication that was the first FDA-approved medication for Fibromyalgia.
Tricyclic, SSRI & SNRI antidepressants: These drugs have the potential to lessen physical pain by changing the neurotransmitter balance in the brain. They often severe double duty as depression is very common due to the low quality of life in comorbid patients.
CBD: In places where CBD is legal it is one of the most popular and widely used pain killers for fibromyalgia.
LDA: Low Dose Abilify has promising preliminary data from the Standford MECFS Clinic as a treatment for fatigue and pain in MECFS.
Benzodiazepines: May be essential for severe ME patients to increase light and noise tolerance, especially in emergencies.
Opioids: Many ME patients are sensitive to opioids including the "atypical" opioid preferred for fibromyalgia tramadol. MCAS patients are strongly contraindicated. Opioid medications are a last resort in fibromyalgia and are generally not effective.
----
Non-Medication Treatment Considerations for Comorbid Patients
Physical therapy and exercise are generally first-line therapies in fibromyalgia. Therefore it is important that patients with both ME and fibro seek out a doctor who understands the barrier of PEM. Some PT may be appropriate for these patients, but only under the supervision of a practitioner who thoroughly understand the dangers. Simply telling the patient to "stop when they feel tired" is not adequate protection. The type of pacing used in autoimmune disease and fibromyalgia is insufficient to protect patients with MECFS. See my post "Pacing is different for MECFS."
However, despite the inability to use PT there are a number of key non-medication therapies for comorbid patients including:
-Heat and Ice Therapy
-Massage Therapy
-Accupuncture or Accupressure
-TENS Therapy
-Non-curative CBT or ACT Therapy
----
Fibromyalgia and MECFS are NOT the same chronic illness.
These two common comorbidities are frequently lumped together as wastebasket diagnoses for patients with chronic fatigue and chronic pain who are too medically complex or undiagnosed. But the truth is that they are their own distinct illnesses, each with their own responses to treatment.
Fibro is an illness defined by widespread severe pain. It often comes alongside dysautonomia fatigue, headache, sleep disturbance and so on, but the key symptom is pain.
In contrast, the key symptom of MECFS properly known as Myalgic Encephalomyelitis and poorly misnamed Chronic Fatigue Syndrome is PEM and PENE aka Post Exertional Malaise and Post Exertional Neuroimmune Exhaustion. This is an exacerbation of all symptoms (pain, fatigue, metabolic, neurologic and immune dysfunction, etc) 24-48 hours after physical or mental exertion. Without PEM there is no ME / CFS.
It is crucial that patients and doctors do not confuse these two diseases. Treatments exist for fibromyalgia. Antidepressant medications can help with the neurologic pain of central sensitization as potentially can treatments like LDN which have an increasingly strong evidence base. Other alternatives to medication like heat therapy, ACT and massage can also be extremely effective.
However, some treatments like GET and CBT that work in fibro can be deeply harmful in MECFS patients. Therefore determining the correct set of diagnoses for yourself or your patient is essential. rheumatologists are particularly prone to medical gaslighting and mistreatment of pwME due to confusion over these diagnoses.
Finally: if you can't diagnose fibro or ME in a patient diagnose idiopathic Chronic Fatigue NOT chronic fatigue syndrome. These are not the same thing. While being undiagnosed or diagnosed with "we don't know" sucks, it is much worse to be thrown in a wastebasket before you receive the testing and diagnosis you actually need and deserve.