Severe ME Awareness Day 8 Things You Need To Know
Severe ME has a spectrum of severity as large as mild and moderate combined.
Severe ME can easily progress to very severe ME, extremely severe ME and death. Most MECFS severity scales do not capture the massive quality of life differences between different levels of severe ME. For example, being able to use social media vs having no social connection to the outside world vs no communication at all is a huge difference. Or needing 24/7 nursing care vs daily household help vs financial assistance. Pain levels and medical needs also vary widely.
See: @m.e_and_more Unofficial Severity Scale and the Hummingbird ME Ability Scale to get a better idea of the full range of MECFS severity.
-------
Severe ME patients are routinely unable to access healthcare.
In many countries home visits from doctors are extremely difficult to arrange or straight up impossible if you are not wealthy. Without access to specialists, GPs, or nursing care many severe patients are left essentially uncared for.
This also makes it very difficult to document the disability caused by the illness and means that when patients must attend hospital for an acute medical emergency or necessary surgery healthcare facilities are horribly prepared to treat and receive these extremely ill patients. This can lead to permanent decline and loss of function following hospital visits.
The inability for severe patients to access healthcare also makes us invisible. Doctors do not understand the extent of severity to which their patients may progress and this leads to inappropriate treatment and dismissal of patient concerns in the mild and moderate patients who can attend clinics.
-------
Severe ME patients are mostly to entirely socially isolated.
The few severe ME patients you see online are in fact generally the most socially active and least sick of the severe patient group. Patients who become very severe tend to be unable to communicate anything besides their most pressing needs to their support team. This makes severe and very severe ME extremely invisible. We disappear from the lives of friends and family, much less being around to meet new people and socialize for fun.
Indeed the reason this post is coming out after severe ME day is because I have been too unwell to raise awareness about severe ME. This is why it is critical that ME advocates most of whom are mild, moderate, or just hitting severe remember to focus attention on very severe and extremely severe patients.
--------
Severe ME patients require and must survive extreme sensory deprivation.
Solitary confinement is known to cause extreme distress, mental health issues and PTSD. But for those with severe and very severe ME it is often necessary treatment. Additionally, we must seek to limit stimuli like light and noise. Few people understand the suffering this level of sensory deprivation and boredom produces.
My room has been carefully designed so that in an instant I can have darkness such that I cannot see my own hand and silence such that noise canceling headphones produce no effect. I am extremely lucky, as I am sometimes able to use some lights and screens with filters and have had the financial resources to create a safe sensory space. For many specialty sleep masks, noise-canceling headphones and earplugs are a constant necessity.
--------
Severe ME affects much more than the patient.
Personally, it affects my:
My husband who had to take a break from pursuing his PhD to care for me 24/7 and sacrifices friends, social life and hobbies
My father who is spending his retirement coordinating my care
My mother, sister and extended family who support me and miss me
My friends who must adjust every activity to my severe limitations and often face months I can barely or not interact with them
Additionally:
We have spent large amounts of money on privately accommodating care I would not otherwise be able to access. For less privileged families, a complete exhaustion of savings and bankruptcy is common.
Severe ME almost certainly has a massively underestimated financial burden on healthcare and disability systems. So many patients I know have been denied disability for ME and receive under other diagnoses or from friends or family often including increasingly aging parents with no alternative. So we are failing to measure and address a massive societal cost.
--------
Severe ME is preventable.
Most people with severe ME lived anywhere from months to decades with mild or moderate ME. The most common cause for progressing to severe is overexertion and illness. It is crucial that people with mild and moderate ME understand the massive danger they face from exertion and identify as immunocompromised taking appropriate steps to minimize infection risk.
People with severe ME often compare becoming severe to when they first became sick. If you have mild or moderate ME think about how much you wish you had known about it before you got sick and wish you had taken the time to fully recover from whatever triggered your ME initially. You have that foresight with regard to severe ME. You might not feel your life with ME is worth preserving but you never recognize what you have until it is gone.
Rest. Pace. Take it seriously. It is much better to do things slower than lose the ability to do them all together.
---------
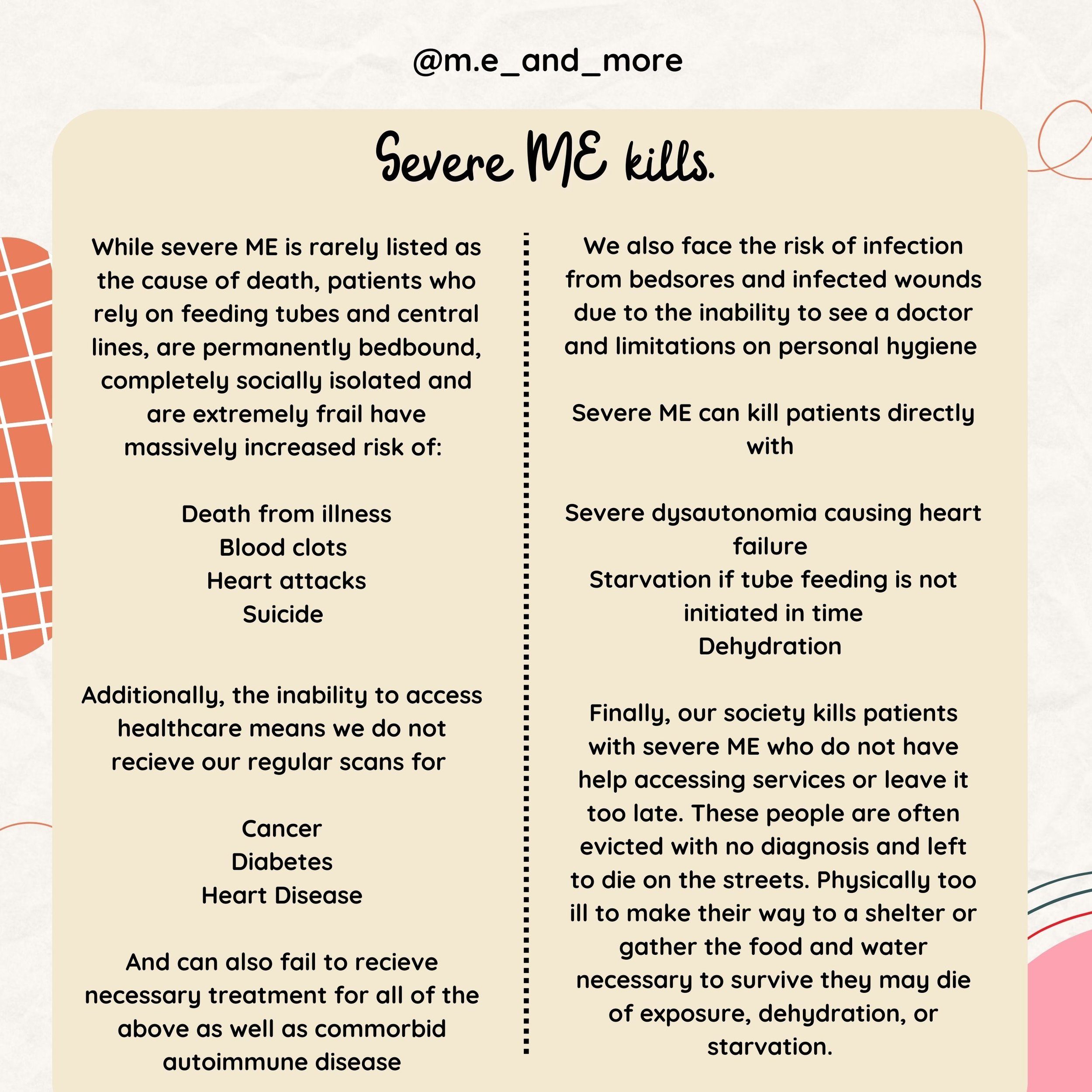
Severe ME kills.
While severe ME is rarely listed as the cause of death, patients who rely on feeding tubes and central lines, are permanently bedbound, completely socially isolated and are extremely frail have massively increased risk of:
Death from illness
Blood clots
Heart attacks
Suicide
Additionally, the innability to access healthcare means we do not receive our regular scans for
Cancer
Diabetes
Heart Disease
And can also fail to receive necessary treatment for all of the above as well as comorbid autoimmune disease
We also face the risk of infection from bedsores and infected wounds due to the inability to see a doctor and limitations on personal hygiene
Severe ME can kill patients directly with
Severe dysautonomia causing heart failure
Starvation if tube feeding is not initiated in time
Dehydration
Finally, our society kills patients with severe ME who do not have help accessing services or leave it too late. These people are often evicted with no diagnosis and left to die on the streets. Physically too ill to make their way to a shelter or gather the food and water necessary to survive they may die of exposure, dehydration or starvation.
---------
Severe ME is not rare.
MECFS affects 0.4-1% people. 25% of those people are severe meaning 100-250 per 100,000. For reference, the most common rare disease multiple sclerosis affects 90 per 100,000 people or less than half as many.
Per patient burden, as measured by disability years of life lost ME is one of the most underfunded diseases in the world. While long covid has brought some funding to ME and post-viral illness it has also increased the patient population massively.
Additionally, severe patients have often struggled in past to participate in the little research that does exist on ME. Studies must be explicitly designed to include severe patients such as sending researchers to patients' houses to collect samples, providing in-home treatment for drug trials, and breaking down tasks into manageable sizes otherwise participation may be impossible for severe patients leading to data that fails to capture a full quarter of the patient population.
---------
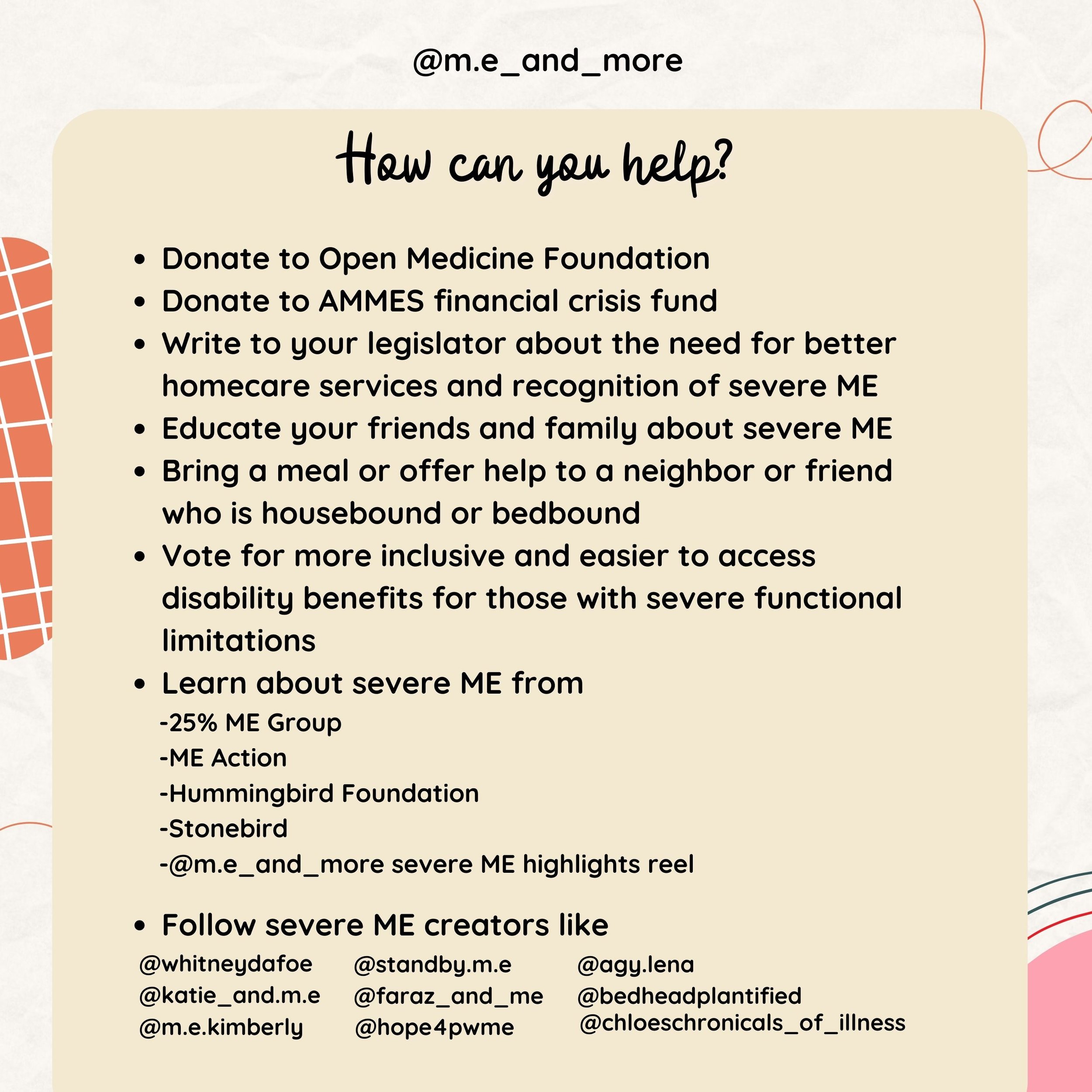
How can you help?
Donate to Open Medicine Foundation
Donate to AMMES financial crisis fund
Write to your legislator about the need for better homecare services and recognition of severe ME
Educate your friends and family about severe ME
Bring a meal or offer help to a neighbor or friend who is housebound or bedbound
Vote for more inclusive and easier to access disability benefits for those with severe functional limitations
Learn about severe ME from
-25% ME Group
-ME Action
-Hummingbird Foundation
-Stonebird
-@m.e_and_more severe ME highlights reel
Follow severe ME creators like
@whitneydafoe
@katie_and.m.e
@standby.m.e
@faraz_and_me
@agy.lena
@bedheadplantified
@m.e.kimberly
@hope4pwme
@chloeschronicals_of_illness
---------
The decision to get a central line or portacath is one of the biggest decisions that people with severe ME face. While port placement can be one of the biggest factors in a patient's recovery, it can also easily incur the life-threatening complication of sepsis.
For me the decision to get a port was easy, my veins could no longer receive IVIG to prevent further neurological degeneration from Behcet's vasculitis.
But for patients who benefit greatly from IVFluids, the decision to get a port often is a balancing act between quality and quantity of life. Risking a chance of death to make your quality of life worth living. While doctors can and should educate patients thoroughly on the risks and benefits of a port, only the patient can really determine whether the risk of sepsis is a worthy trade-off for the improvement in health.
This post aims to share as much of what I have learned in the past 3 months of working to get a port. While ports are the topic of this post, much of it applies to central lines of any sort. I highly recommend if you are interested in getting a port, PICC, or hickman that you join some Facebook groups about central lines so you can better understand the reality of living with these devices. My tips and advice are directly based on my (quite positive so far) experience. Others may feel differently and have different advice.
For example, some people cannot wear a bra at all when their port is new or even when it is healed. But others find wearing a well-fitted bra essential to comfort when they are healing from surgery.
Myalgic Encephalomyelitis is a severe illness and very Severe ME can be deadly. It is essential that doctors understand how sick patients with MECFS can be because otherwise, they may fail to prescribe patients with appropriate treatment due to their belief that the treatment is riskier than the disease or they don't believe the patient's suffering is worthy of palliative care.
Just as ambulatory wheelchair users may benefit greatly from a chair despite being able to walk short distances, pwME may benefit greatly from a port even if they can drink and eat orally so long as they are unable to meet their hydration and nutrition needs. While the decision to get a central line should never be taken lightly, it is inappropriate to deny medical intervention until the condition becomes life-threatening. No patient should be forced to starve or dehydrate to the point of delirium solely so a doctor can feel that their patient "proved" the need for an intervention. First Do No Harm does only mean not only apply to the active decision to provide treatment, but also the passive decision to allow patient suffering and disease progression by denying effective treatment.