Sleep & Myalgic Encephalomyelitis : Treatment Options Explained.

Common sleep issues in ME
Sleep dysfunction is part of international consensus criteria for myalgic encephalomyelitis and sleep dysfunction in ME is common. This can take the form of:
-Unrefreshing Sleep: A part of fatigue, when patients sleep they do not feel refreshed or less tired upon waking.
-Reversed Phase Sleep Cycle: Patients sleep during the day and are awake at night. For example, waking up at 6 p.m. and going to bed at 6 a.m.
-Hypersomnia: Patients sleep much more than 8 hours a night. They may sleep 12 hours, 16 hours or have trouble maintaining consciousness.
-Insomnia: Patients are unable to sleep, sometimes for days at a time.
Patients may also switch between periods of hypersomnia and insomnia and all of these sleep dysfunctions can co-occur within a single patient.
—-
Accommodating Reversed Phase Sleep Cycle
Because pacing is extraordinarily difficult when sleep is disrupted it can be advisable for patients with reversed phase sleep cycles to simply keep this schedule. Unfortunately, this may not always be possible if caregiving is only available during the day.
It is not particularly important if a patient sleeps at strange hours but it is important for patients to try to keep a consistent sleep routine with at least 8 hours of time every day where they will either sleep or attempt to sleep.
Traditional sleep training where patients force themselves to stay awake to get onto a sleep schedule is unadvised as it may cause crashes.
—-
Hypersomnia Treatment Options
Warning: Hypersomnia particularly in severe and very severe patients is often a survival coping mechanism to preserve energy. Thus treating hypersomnia must be done with a keen eye towards pacing and considered a reduction in resting time.
-Caffeine: The most easily accessible medication to treat hypersomnia is caffeine. This is a good test of whether your hypersomnia responds well to additional stimuli. Caution should be used and small doses to start.
-Stimulant Medications: If the response to caffeine is good or caffeine is not an option, stimulant medications can be tried. However, it should be noted that patients have reported loss of function following treatment with stimulants as they block the body's natural cues for pacing making overexertion easy. Therefore, they should be used only with extreme caution and very careful monitoring and pacing.
—-
Insomnia Treatment
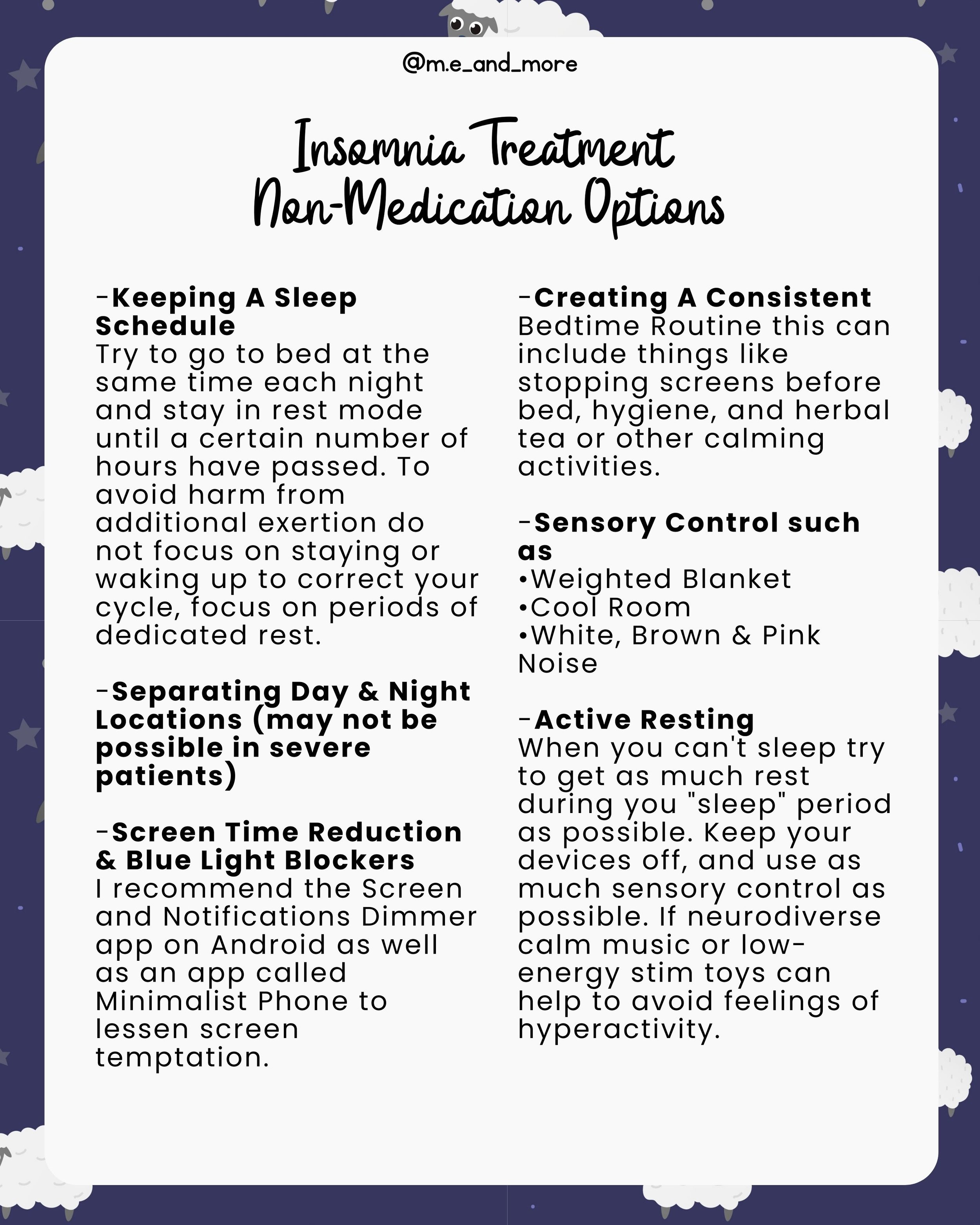
Non-Medication Options
-Keeping A Sleep Schedule
Try to go to bed at the same time each night and stay in rest mode until a certain number of hours have passed. To avoid harm from additional exertion do not focus on staying or waking up to correct your cycle, focus on periods of dedicated rest.
-Separating Day & Night Locations (may not be possible in severe patients)
-Screen Time Reduction & Blue Light Blockers
I recommend the Screen and Notifications Dimmer app on Android as well as an app called Minimalist Phone to lessen screen temptation.
-Creating A Consistent Bedtime Routine this can include things like stopping screens before bed, hygiene, and herbal tea or other calming activities.
-Sensory Control such as
•Weighted Blanket
•Cool Room
•White, Brown & Pink Noise
-Active Resting
When you can't sleep try to get as much rest during you "sleep" period as possible. Keep your devices off, and use as much sensory control as possible. If neurodiverse calm music or low-energy stim toys can help to avoid feelings of hyperactivity.
—-
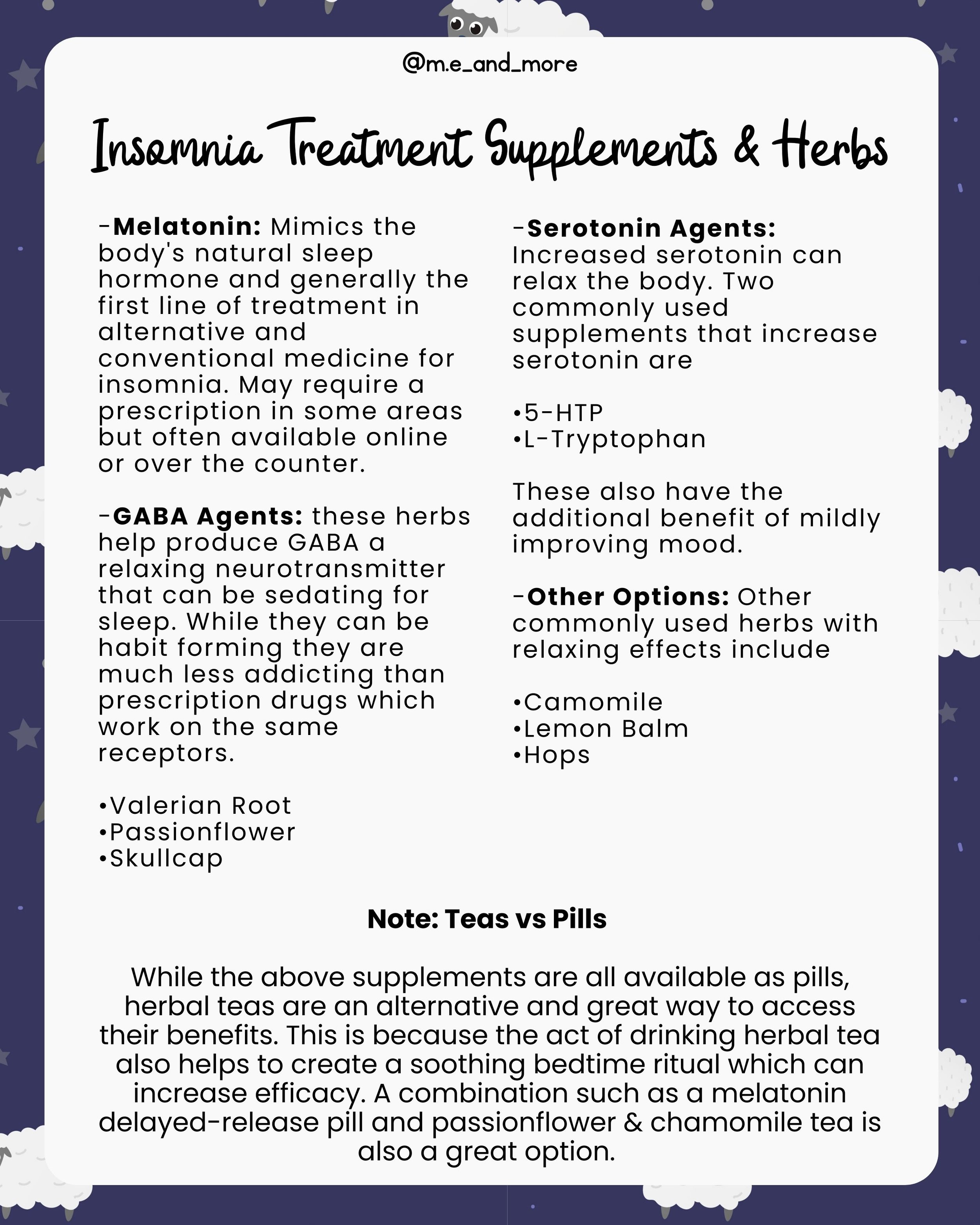
Insomnia Treatment Supplements & Herbs
-Melatonin: Mimics the body's natural sleep hormone and generally the first line of treatment in alternative and conventional medicine for insomnia. May require a prescription in some areas but often available online or over the counter.
-GABA Agents: these herbs help produce GABA a relaxing neurotransmitter that can be sedating for sleep. While they can be habit forming they are much less addicting than prescription drugs which work on the same receptors.
•Valerian Root
•Passionflower
•Skullcap
-Serotonin Agents: Increased serotonin can relax the body. Two commonly used supplements that increase serotonin are
•5-HTP
•L-Tryptophan
These also have the additional benefit of mildly improving mood.
-Other Options: Other commonly used herbs with relaxing effects include
•Camomile
•Lemon Balm
•Hops
Note: Teas vs Pills
While the above supplements are all available as pills, herbal teas are an alternative and great way to access their benefits. This is because the act of drinking herbal tea also helps to create a soothing bedtime ritual which can increase efficacy. A combination such as a melatonin delayed-release pill and passionflower & chamomile tea is also a great option.
—-
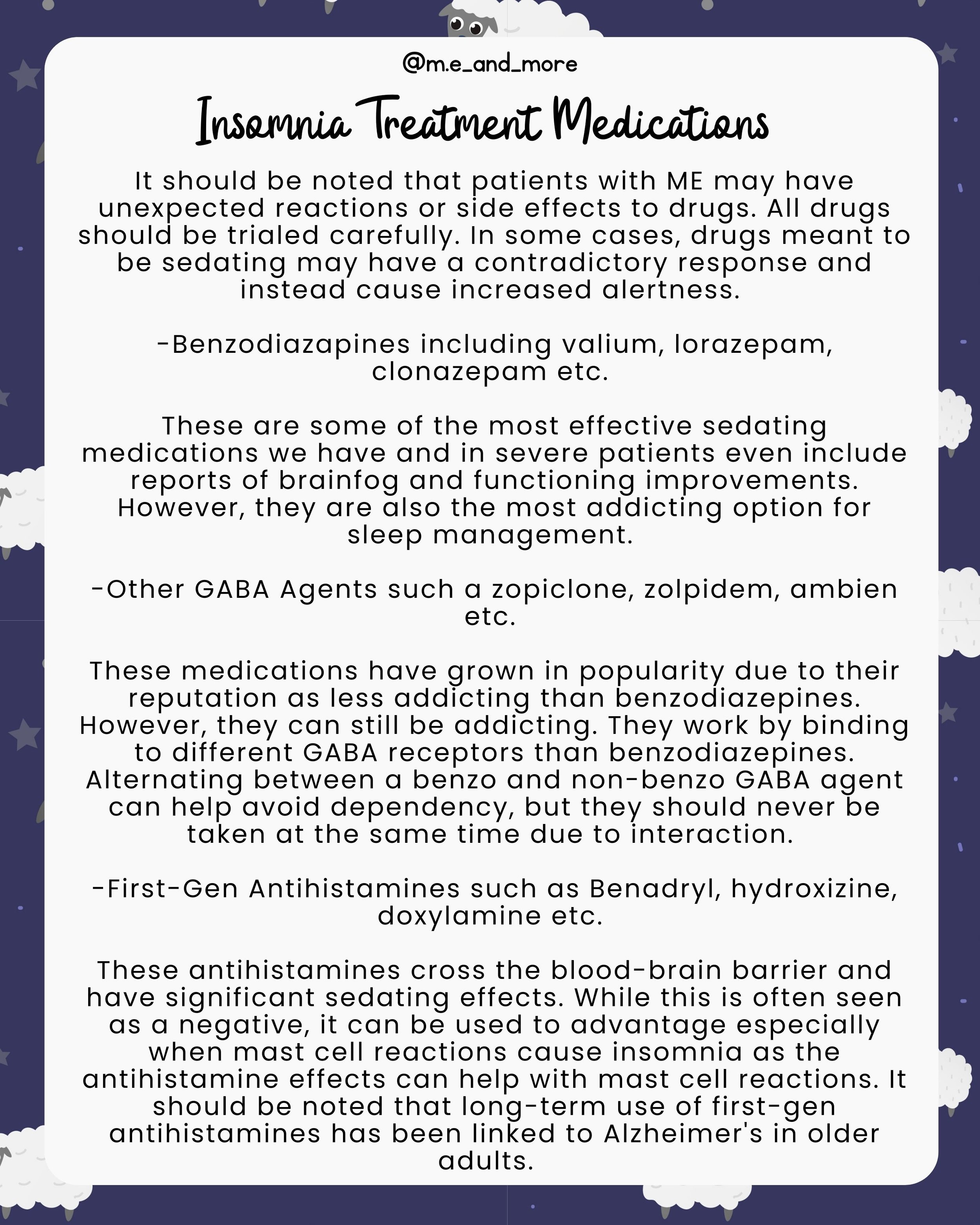
Insomnia Treatment Medications
It should be noted that patients with ME may have unexpected reactions or side effects to drugs. All drugs should be trialed carefully. In some cases, drugs meant to be sedating may have a contradictory response and instead cause increased alertness.
-Benzodiazapines including valium, lorazepam, clonazepam etc.
These are some of the most effective sedating medications we have and in severe patients even include reports of brainfog and functioning improvements. However, they are also the most addicting option for sleep management.
-Other GABA Agents such a zopiclone, zolpidem, ambien etc.
These medications have grown in popularity due to their reputation as less addicting than benzodiazepines. However, they can still be addicting. They work by binding to different GABA receptors than benzodiazepines. Alternating between a benzo and non-benzo GABA agent can help avoid dependency, but they should never be taken at the same time due to interaction.
-First-Gen Antihistamines such as Benadryl, hydroxizine, doxylamine etc.
These antihistamines cross the blood-brain barrier and have significant sedating effects. While this is often seen as a negative, it can be used to advantage especially when mast cell reactions cause insomnia as the antihistamine effects can help with mast cell reactions. It should be noted that long-term use of first-gen antihistamines has been linked to Alzheimer's in older adults.
—-
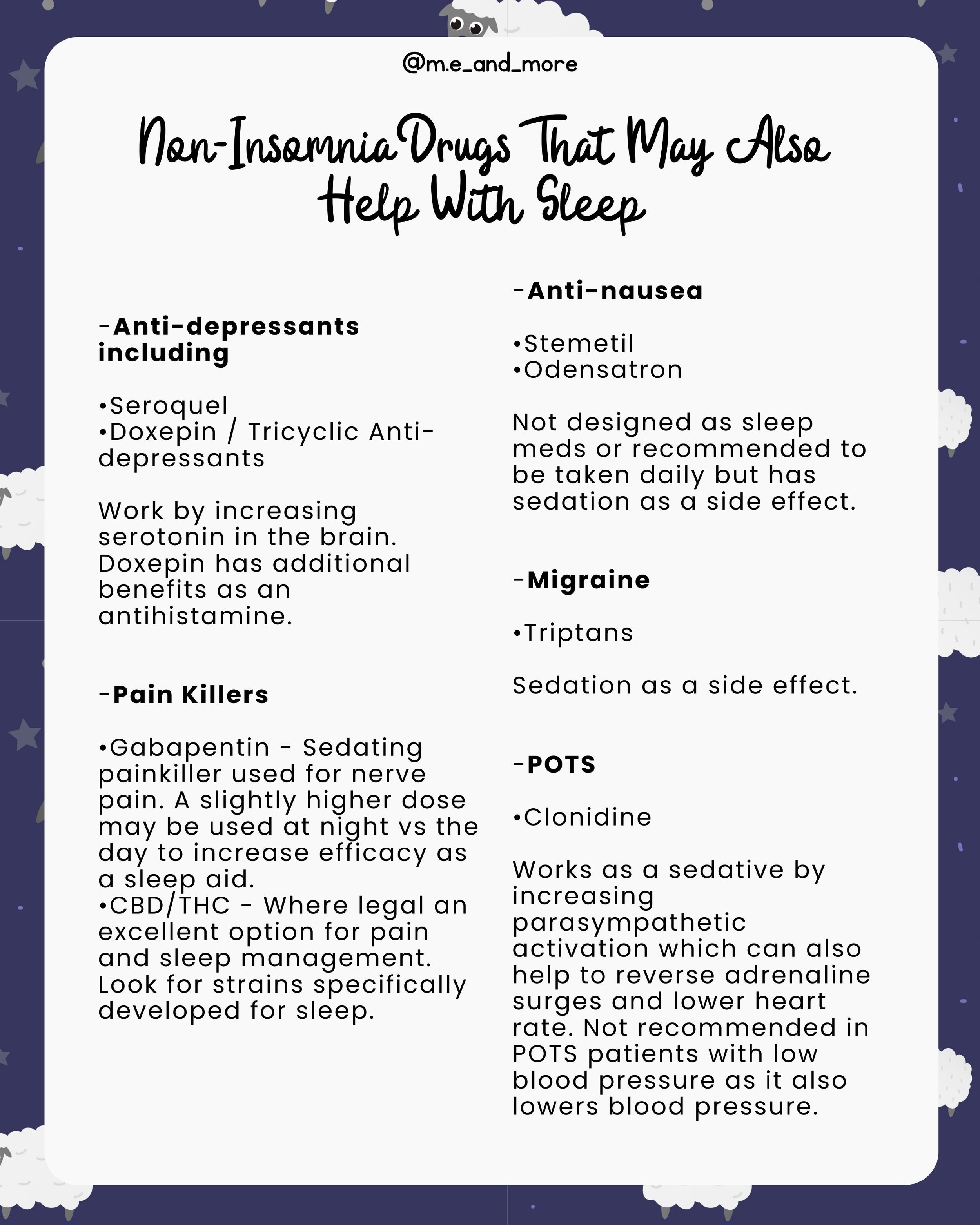
Non-Insomnia Drugs That May Also
Help With Sleep
-Anti-depressants including
•Seroquel
•Doxepin / Tricyclic Anti-depressants
Work by increasing serotonin in the brain. Doxepin has additional benefits as an antihistamine.
-Pain Killers
•Gabapentin - Sedating painkiller used for nerve pain. A slightly higher dose may be used at night vs the day to increase efficacy as a sleep aid.
•CBD/THC - Where legal an excellent option for pain and sleep management. Look for strains specifically developed for sleep.
-Anti-nausea
•Stemetil
•Odensatron
Not designed as sleep meds or recommended to be taken daily but has sedation as a side effect.
-Migraine
•Triptans
Sedation as a side effect.
-POTS
•Clonidine
Works as a sedative by increasing parasympathetic activation which can also help to reverse adrenaline surges and lower heart rate. Not recommended in POTS patients with low blood pressure as it also lowers blood pressure.
—-
Insomnia Medication,
Stigma & Addiction
Insomnia medication can be addictive. There are some things that can be done to prevent this such as:
-Taking periodic breaks from medication or only taking it on nights you already have struggled to sleep.
-Rotating between medications.
-Alternating medications and supplements.
However, even if you cannot avoid medication dependency this doesn't mean you shouldn't use it.
ME is a lifelong illness for the vast majority of people. As such a lifelong dependency on medication should not stop you from improving the quality of your life with ME. If you truly do experience remission being able to stop medications will be a problem you will be thankful to have.
There is a difference between being dependent on a medication to manage chronic symptoms and being addicted to a medication for emotional reasons. Both are legitimate medical problems, but only in the case of a mental addiction to medication is it helpful to try to avoid taking it.
—-
Adrenaline Cycles & Insomnia
Adrenaline frequently appears during crashes. Using that adrenaline to do exciting things will only increase the amount of adrenaline present. For people with ME, even activities like watching television can be exciting and high adrenaline.
Therefore, in addition to the dangers traditional sleep training poses to pacing, it is also often a very ineffectual strategy for battling insomnia since forcing yourself to stay awake will only feed the adrenaline surge.
Instead, the goal should be to stop the adrenaline surge as quickly as possible by resting aggressively. This means doing as little as you possibly can while staying alive, ideally resting in a dark and quiet room with no stimuli.
—-
Sleep is essential for health. Yet one of the hallmark symptoms of Myalgic Encephalomyelitis aka ME / CFS an Energy Limiting Chronic Illness that causes severe chronic fatigue is sleep dysfunction.
⠀
So what can we do to stop poor sleep from draining our already limited health and energy?
⠀
Sleep management is one of the most important areas of symptom management for any doctor treating someone with ME. Indeed, disrupting your sleep is one of the main reasons to seek help for any symptom be it chronic pain, nausea, tachycardia etc.
⠀
Thankfully there are many ways to adress sleep dysfunction and promote restful sleep from sleep hygiene like
⠀
-Establishing a bedtime routine
-Keeping your room cool and comfortable
-Avoiding blue light before bed
⠀
To supplements like melatonin, valerian, and passion flower and of course sleep medications like zopiclone and benzodiazapines.
⠀
While supplements and medication in particular do carry risk of dependency, improving sleep is one of the most crucial elements of improving quality of life for those with ME and complex chronic illness.
⠀
Because these diseases are chronic, long term medication use is often unavoidable. While using the minimum effective dose, rotating medications and supplements, and focusing on non-medication interventions first is important, the most important thing is establishing regular and effective sleep patterns. This will help control all other symptoms, assist with pacing, and can drastically improve quality of life.
⠀
While fatigue is defined by unrefreshing sleep, this does not negate the importance of getting the best sleep possible. I sincerely hope that this guide can assist in that endeavor.
⠀
Comment and share what has helped you sleep better with MECFS!
⠀
Millions missing millions more long covid, long chronically ill, spoonie, spoonie community NEIS Void.
⠀
Disclaimer: this post is not intended as medical advice and I am not a doctor. Please discuss all supplement and medication use with your primary physician.